You should regularly perform a breast check-up in order to notice any changes to your breast’s health. But should you just perform a breast check-up yourself or should you get a doctor to do it? The answer is both.
You know your own body better than anyone else, so you will be the first to notice any pain or changes to your breast. Although, a doctor’s breast examination will be much more thorough and it will provide you with peace of mind regarding the results.
If you are concerned about any breast symptoms, it is always advisable to contact your GP immediately. In this article we’ll explain how to perform regular self breast check ups and why you should schedule a doctor’s appointment about your breast health.
Self breast check up
The best way to remain aware of any changes to your breasts is to perform regular self check ups. You should know how your breasts usually feel so that you can take note of any sudden changes.
It’s normal for some women to have naturally lumpy breasts especially near the armpit. After menopause, breasts also tend to feel softer, less firm and not as lumpy. It’s important to feel your own breasts and know what’s normal for you.
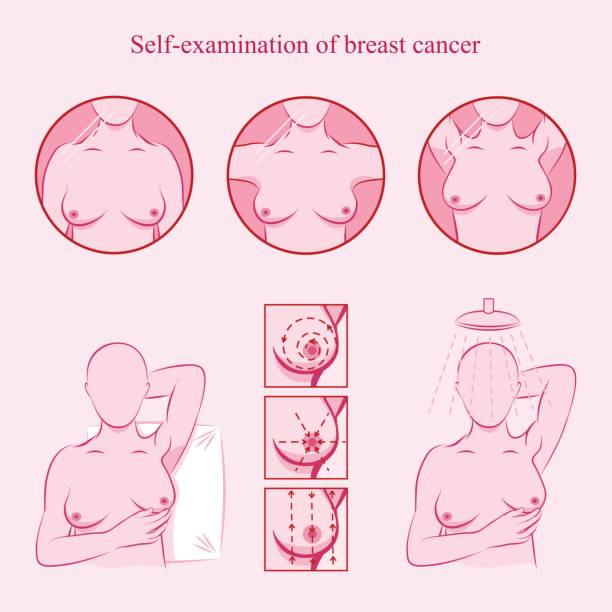
How to perform a self breast examination?
Use your fingers and apply medium pressure to your breasts, ensure that you check for any lumps in the whole breast, armpit and all the way up to the collarbone. You should also look at your breasts in the mirror, raising your arms above your head and checking them from all angles.
How often should I perform a self breast check up?
It is recommended that you perform a self breast check-up once a month. You should aim to perform this check up on the same day of every month and ideally 3-4 days after your period has begun.
Doctors breast check up
A breast check up with your doctor or a breast specialist is the best way to reassure yourself if you are experiencing any changes to your breasts or if you are concerned about your potential risk of developing breast cancer. They will assess you and your individual circumstances, giving you a definitive answer regarding your breasts health.
You will automatically be invited for breast screening by the NHS if you are female and between the ages of 50 and 53. Then you’ll be invited every 3 years until you turn 71. However you should arrange to see a doctor or breast specialist before then if you are concerned.
When should I see my doctor about my breasts?
If you experience any of the following symptoms, ensure that you arrange for a breast check up with your GP or breast surgeon specialist. The symptoms to look out for include:
- Changes within the breast’s texture, e.g.) thickening of the breast’s tissue.
- Changes to the breast’s skin, e.g.) dimpling
- Sudden changes to the breast’s size and shape.
- A lump found within the breast or armpit.
- Nipple changes, e.g.) an inverted or retracted nipple.
- Redness of flaky skin around the nipple area.
- Discharge or blood coming from the nipple, not breast milk.
- Breast or armpit pain.
- Swelling in your armpit or swelling near your collarbone.
If you are experiencing any of these symptoms, it’s most likely not breast cancer, but nonetheless it is important to get them checked out for reassurance and peace of mind.
Should I get a mammogram as part of my breast check up?
A mammogram is an x-ray of the breast and for many women, it is the most efficient method for detecting breast cancer early, before it is big enough to cause symptoms for you to feel a lump. Your doctor may recommend a mammogram following an initial breast examination if they feel it is necessary.
It is also recommended that women aged 50 to 70, who are at an average risk for developing breast cancer, should get a mammogram every three years. If you have had a history of breast cancer, it is advised that you get one once a year for five years after your diagnosis and then every three years thereafter..
Your doctor will advise you on the most appropriate solution.
Can a doctor determine my risk of developing breast cancer?
Due to genomic medicine, doctors and breast specialists are now able to perform tests that analyse the individual’s DNA to determine their risk of developing breast cancer. There are two tests that your surgeon may be able to carry out:
Invitae BRCA STAT Panel
An Invitae BRCA STAT Panel can detect the presence of BRCA1 or BRCA 2 genes within an individual. These are rare gene defects that can significantly increase an individual’s risk of developing breast cancer.
This test is used for individuals that have a strong family history of developing breast cancer. It may also be used for women who have previously had breast cancer and want to know if they are at risk of developing it in their other breast.
AnteBC Test
This AnteBC Test is recommended for women between the ages of 30 and 75. It is suitable for women who do not have a family history of breast cancer but wish to know their risk of developing breast cancer at some point in their life.
The determined score does not definitively indicate whether or not a person will experience breast cancer, it only predicts their chances of potentially developing it.
The importance of getting a breast check up
It is very important to regularly perform a breast check up on yourself and to schedule a doctor’s appointment when appropriate and necessary. Paying regular attention to changes in your breasts means that any diagnosis can be treated early and more effectively.
For peace of mind and reassurance, check your breasts yourself and get a breast check up. If you would like to arrange for a breast check up with a breast surgeon specialist, you can do so here.








